PRI has considerable interest in formularies as they replace physician judgment in the selection of appropriate medicines. For prior posts on formularies, see “A Primer on Formularies” and “Who Should Decide?” Treating doctors believe that they are the best judges of the treatment needed and the medicines required for their patients.
Formularies are a standard feature in health insurance and now are appearing in the workers compensation area. In health insurance policies, there are “tiers” of medicines where the insured individual pays a different co-pay depending on the “tier.” Generally, the more expensive medicines are in the upper “tier” requiring the largest co-pay which, in many cases, is unaffordable for most people.
In the workers compensation world, the issue of formularies is different. Since an injured worker is not required to contribute a co-pay, the health insurance matrix is not applicable. A workers compensation formulary is typically a list of preferred medicines that can be prescribed without prior authorization. Medicines which are not preferred typically need to be “pre-authorized” in order to be covered.
Treatment guidelines are sometimes connected to formularies. In medicine, treatment guidelines are frequently decided by medical specialists, usually under the aegis of the American Board of Medical Specialties (ABMS). These “treatment guidelines” are agreed to by treating doctors and they are almost uniformly accepted by organized medicine. At one time – prior to recent federal budget cuts – a federal agency known as the National Guideline Clearing House (NGC) was the “gold standard” for treatment guidelines and it recognized any number of treatment guidelines for multiple conditions. The NGC would either certify of reject proposed treatment guidelines.
Within the workers compensation space, a package of treatment guidelines/formularies is being sold by two companies. MGC Health, part of the Hearst Health Network, offers a subscription based product known as the Official Disability Guidelines (ODG). The other vendor is the Reed Group, a subsidiary of Guardian Life Insurance Company, which publishes MDGuidelines and these guidelines are developed by the American College of Occupational and Environmental Medicine (ACOEM). Both MGC Health and Reed are actively involved in “selling” their products to individual states and doctors in those states may “subscribe” in order to know the rules of treatment and the allowable medicines.
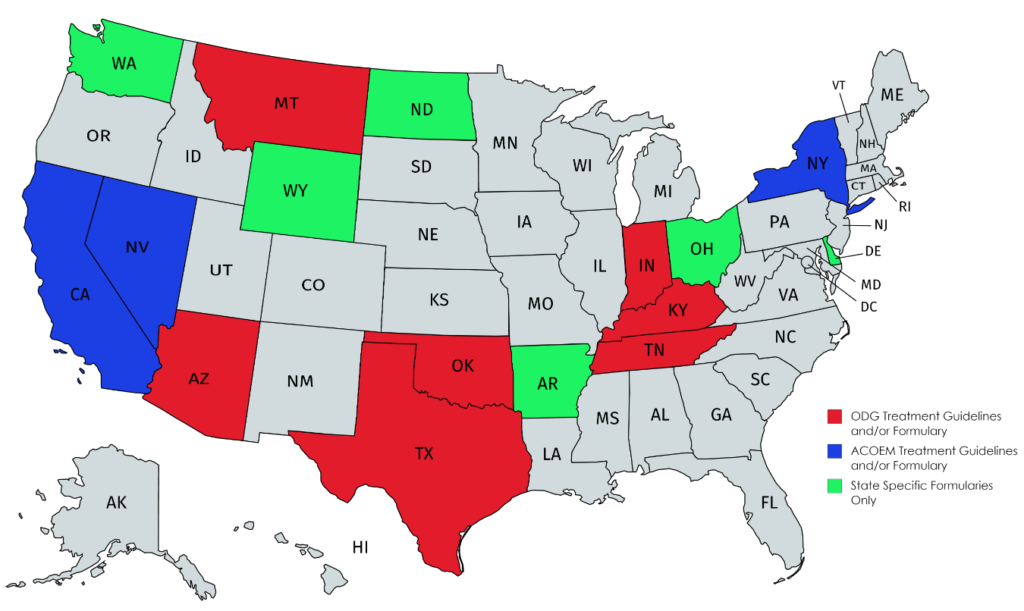
At the present time, 16 states have workers compensation formularies and/or treatment guidelines which means the doctor must prescribe the medicine listed on the formulary and following the prescribed guidelines unless the doctor wishes to seek special approval. Of the 16 states, 7 follow the ODG formulary, 3 follow the ACOEM formulary and 6 are state specific. In approximately half of these states, there is only a formulary without associated treatment guidelines.
A review of the literature indicates that ODG makes the most extravagant claims about the efficacy and scientific basis of its treatment guidelines/formulary.
Whether ODG, ACOEM or a state specific formulary, the principal reason for adoption is cost containment. Since pharmaceutical costs are a relatively minor part of total workers compensation claim expenses, the adoption of treatment guidelines/formularies seems to have little effect on the overall cost of insurance.
The question remains: Do treatment guidelines and formularies work? The answer seem to be both yes and no.
CLAIM NUMBER 1: ODG claims that it substantially reduces workers compensation insurance costs and points to the states where the ODG Treatment Guidelines/Formulary have been adopted as proof of this claim. This is ODG’s most extravagant and questionable claim. Workers compensation insurance rates have been falling like a stone in all states including non-formulary states. The principal reason for this is a continuing decline in claim frequency with the corresponding decrease in medical costs and claims for lost income. Indeed, since 2006 the National Council of Compensation Insurance recently has reported that claims are down 30%.
ODG points to Texas and Tennessee which adopted its treatment guidelines/formulary but Maryland and Virginia are similarly inexpensive (and even less than Tennessee) even though neither state has adopted treatment guidelines/formularies and the ODG formulary state of Montana is substantially more expensive than most states. The cost of workers compensation insurance in the various states can be seen by reviewing the Oregon Report which is generally acknowledged to be the most accurate ranking of state costs.
CLAIM NUMBER 2: ODG claims that it substantially reduces the use of opioid medicines and points to Tennessee. However, according to the Tennessee Board of Workers’ Compensation Annual Report 2019 (see below), while there was a decrease of 16% in the use of opioids, this reduction was experienced in non-formulary states also.
“Opioid Reduction
It was expected that use of the ODG formulary would lead to the reduction of opioid prescriptions in the workers’ compensation system in Tennessee. There was a decrease of 16% in the use of opioids in NCCI’s study period. However, this reduction was experienced in non-formulary states also.”
Indeed, opioid prescriptions have been decreasing since 2013 as has been regularly reported by major workers compensation pharmacy benefit managers (PBMs). For a chart reviewing the decline from 2013 through 2016, see here.
The principal reason for dramatic opioid reduction was that doctors cut back on writing new prescriptions as it became clear that there was a substantial opioid addiction problem. It was the change in prescription practices that ended an excessive reliance on opioids and, as noted by the National Council on Compensation Insurance, “the ODG Formulary had a limited observed impact on opioid utilization ….”
CLAIM NUMBER 3: The treatment guidelines associated with the medicine formulary are “evidence-based” and scientifically valid. This is a claim made by both ODG and ACOEM. In 2017, the Rand Corporation reviewed the ODG treatment guidelines. In technical quality, Rand gave ODG a 58% rating out of a possible 100%, a failing grade in any school. In clinical acceptance, Rand gave ODG a “fair/good” rating. The principal criticism was that the ODG guidelines were, in many cases, not “evidence-based” at all and not supported by peer reviewed literature.
The Reed guidelines are developed by the American College of Occupational and Environmental Medicine and these guidelines are peer reviewed. One caveat: ACOEM is not a recognized specialty of the American Board of Medical Specialties (ABMS). ABMS certifies appropriate specialties of medicine so, while ACOEM is “peer reviewed,” it would appear that ACOEM’s senior leadership are doctors employed by large corporations.
CLAIM NUMBER 4: Formularies save money on prescription costs. While costs in formulary states may decrease, the question is how much of this can be attributed to formulary implementation versus other factors such as state mandated regulations requiring the use of generic medications, declining claim frequency, use of networks, and similar factors. One question is who collects the saved money?
In most cases, the formulary is administered by a company known as a PBM. To say the least, the role of PBMs is controversial as it’s not clear that PBMs choose the “best” medicine as opposed to the medicine where the PBM can get the best deal either for its client or for itself. Ohio recently brought a lawsuit against its PBM (Optum) claiming that Optum had secured itself a $16 million profit that should’ve accrued to the state. Optum no longer handles Ohio’s program.
Criticism of PBMs is widespread throughout the country and not just in the workers compensation area. Ohio now believes that Medicaid PBMs have overcharged the state more than $240 million.
The controversy about PBMs has resulted in hundreds of laws aimed at reform. The National Conference of State Legislators has a compendium of these various laws
CLAIM NUMBER 5: ODG claims that it substantially reduces utilization of those drugs which are not on the approved list for the formulary. Similar claims are made by the state specific formularies.
It is axiomatic that utilization of “N” medicines will drop as a result of a closed formulary. Indeed, the whole purpose of the formulary is to encourage doctors to choose “Y” medicines and to avoid “N” medicines which require prior authorization from claims personnel. The real question, however, is whether the “N” medicine is more appropriate and necessary for the injured worker. Proponents of formularies do not answer that question.
CONCLUSION
The choice of ODG versus ACOEM appears to be a matter of politics as much as anything else. ODG has been selected in “Red” states where Republicans control the legislature and where business and insurance interests are more dominant. The ODG states seem less concerned about whether the guidelines are “peer reviewed” and more interested in cost cutting.
ACOEM has been selected in “Blue” states where Democrats are in control and where the medical community and organized labor receive greater attention and where “peer review” is deemed important as insuring quality care.




