49 states (Missouri still out) and the District of Columbia have established Prescription Drug Monitoring Programs (PDMP) which track certain schedule drugs and provide a database which can be accessed by doctors, licensing authorities and law enforcement. While such efforts began in New York as early as 1919, it was only with the advent of computers that a comprehensive program could be developed and accessed. In addition, computer technology allows for “real time” information to be shared.
While PDMPs were not initiated by medical interests, they are of tremendous value to doctors, particularly those who are operating in settings where pain management is involved. The ability of a doctor to determine whether a particular patient is “doctor shopping” for opioids is invaluable and allows for intervention in a particular case.
PRI conducted a survey to determine the status of state PDMPs. In approximately 10 states, “batching” is allowed which means that a doctor’s office could send a request for information on the 10 patients to be seen in the next day and receive a response from the PDMP. This saves considerable administrative time over the normal requirement that a request to a PDMP must be on a single person basis. Consult the PRI Model Legislation module for a proposal to require “batching”.
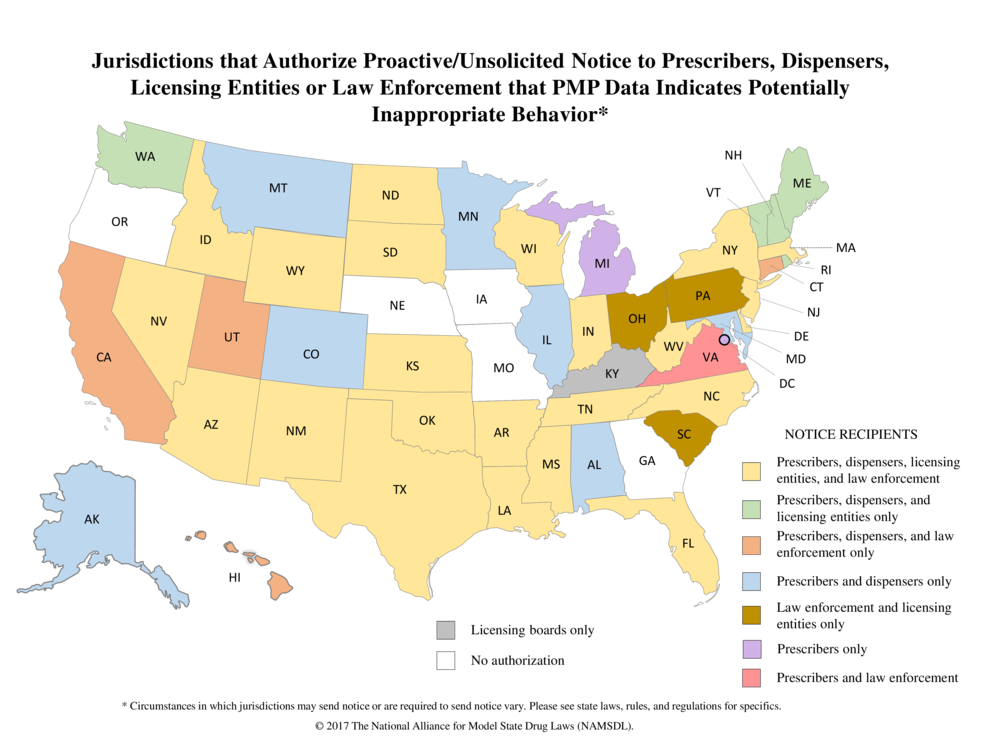
Depending on the state, the PDMP will alert participants to situations that need to be addressed. In several states, however, the “alert” goes only to licensing authorities or law enforcement. It should be obvious that the alert should go to the doctor first so that he or she could take corrective action if necessary. Most PDMPs were initiated by law enforcement and doctors were not initially consulted. However, in all state PDMPs, doctors are given access and PRI believes that doctors should be given “alerts” first as well. Accordingly, the statutes in the states of Ohio, Pennsylvania, South Caroline and Kentucky and should be amended to include doctors in the “alert” function. Moreover, “alerts” should be sent to doctors in Nebraska, Iowa, Oregon and Georgia which, at the present time, do not have an “alert” function.
Below is a 50 state map showing the groups who are “alerted” when the PDMP detects an anomaly. This map is the work of the National Alliance for Model State Drug Laws (NAMSDL) and its CEO, Sherry Green, and is used with their permission.
1211 Cathedral Street, Baltimore, Maryland 21201 – Call Our Offices – 443.449.2287
1211 Cathedral Street, Baltimore, Maryland 21201 – Call Our Offices – 443.449.2287